
One example designed to assess independence in both basic and instrumental ADLs is the Activities of Daily Living Questionnaire (ADL-Q ), which provides an overall indication of functional independence, as well as, more specific assessment of targeted domains (e.g., self-care, household care, employment and recreation, shopping and money, travel, and communication). Given variable levels of insight among individuals with neurodegenerative disease, assessment of functional independence often uses collateral reports. Although performing ADLs involves multiple cognitive processes, research suggests that levels of executive functioning may be particularly important in predicting levels of functional impairment. In the dementia process, ADLs are typically lost in a hierarchical manner, with instrumental ADLs being impacted before basic ADLs.
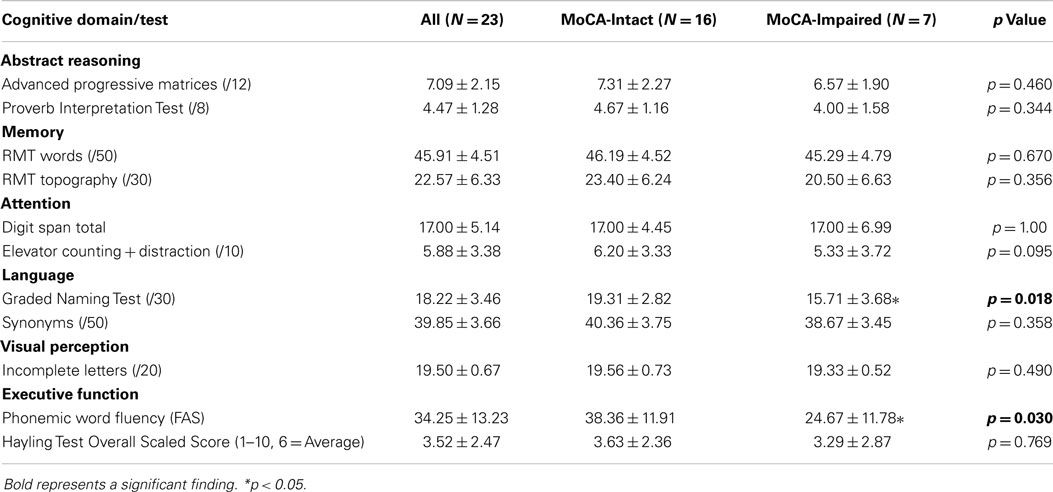
Research comparing performance on brief cognitive screening tests and measures of ADLs has demonstrated that individuals with greater cognitive impairment are more likely to have functional impairments in ADLs (e.g.,, ). Clinicians often use brief cognitive screening tests (e.g., Montreal Cognitive Assessment, Mini-Mental Status Examination) and measures of ADLs as part of routine dementia evaluations, and understanding how such measures are related is important to establish how performance on cognitive screening may be predictive of functional independence and establish the need for further testing.
Measuring an individual's functioning in ADLs is an important aspect of assessment for neurodegenerative disease and is necessary in making accurate diagnoses, evaluating the severity of disease, monitoring disease progression over time, and ensuring appropriate levels of support are in place. Impairments in basic and instrumental activities of daily living (ADL) are often associated with cognitive decline in elderly populations.


 0 kommentar(er)
0 kommentar(er)
